On March 31, the ImmunizeBC website will move over to HealthLinkBC.ca After this date, you will be automatically redirected to HealthLink BC’s Immunization landing page. HealthLink BC provides trusted health information online and over the phone 24 hours a day, seven days a week by calling 8-1-1.
Date last reviewed:
Thursday, Feb 27, 2025
HealthLinkBC
Available in عربى (Arabic), Français (French), یسراف (Farsi), 한국어 (Korean), ਪੰਜਾਬੀ (Punjabi), and other languages.
Diseases it protects against
The MMR vaccine protects against:
- Measles
- Mumps
- Rubella
These diseases can cause serious illness, hospitalization, and even death. Learn more about these diseases.
In Canada, measles, mumps, and rubella vaccines are only available as the combination MMR vaccine and measles, mumps, rubella, varicella (MMRV) vaccine.
Alert
Measles cases are rising worldwide
Check your immunization records and make sure your family is protected against measles, especially if travelling.
Who should get the MMR vaccine
| Age | Schedule |
|---|---|
| Infants & young children |
|
| School-age children & teens |
|
| Adults |
|
Fact
Did you know?
Measles is so contagious that if one person has it, 9 out of 10 people around them will become infected if they are not protected.
Safety
Vaccine safety is a top priority in Canada. Every vaccine must be shown to be safe and effective before it is approved for use in Canada. After approval, the safety of vaccines is continuously monitored. Learn more about vaccine safety.
Fact
Vaccines are very safe.
Getting the vaccine is much safer than getting one of the diseases.
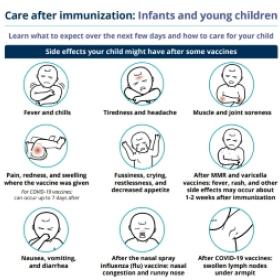
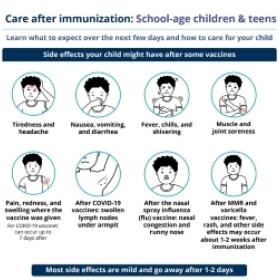
Side effects
Many people have no side effects from vaccines. For those that do, they are usually mild and go away on their own within a few days. Serious side effects are very rare.
Common reactions to the MMR vaccine may include:
- Soreness, redness and swelling where the vaccine was given.
- Fever, headache, muscle soreness, nausea.
- A rash that looks like measles and swelling of glands in the cheeks or neck can occur about 7 to 12 days after getting the vaccine.
- Temporary joint pain may occur in teenage and adult women.
In rare cases, more serious reactions can occur. These can include seizures caused by fever (about 1 child in 3,000), a temporary drop in the blood cells that help prevent bleeding (about 1 person in 30,000), and encephalitis, which is inflammation of the brain (about 1 person in 1 million). It's important to note that the possibility of getting encephalitis from measles is about 1 in 1,000, which is much higher than from the vaccine.
It is important to stay in the clinic for 15 minutes after getting any vaccine because there is an extremely rare chance of a life-threatening allergic reaction called anaphylaxis. If this reaction occurs, your health care provider is prepared to treat it.
Let your immunization provider/clinic or health care provider know if you or your child have any serious or unexpected side effects after immunization.
How to manage side effects
For information on how to manage side effects, view the immunization aftercare sheets below.
Who should not get the vaccine
Speak with your health care provider if you or your child:
- Have had a life-threatening reaction to a previous dose of measles, mumps, or rubella vaccine or any component of the vaccine, including gelatin or neomycin.
- Have an immune system weakened by disease or medical treatment.
- Have had a drop in platelets, the blood cells that help prevent bleeding, after getting a previous dose of MMR vaccine without another cause being identified.
- Have had a blood transfusion or received other blood products within the past 12 months.
- Are pregnant or planning to become pregnant. People should avoid becoming pregnant for 1 month after getting the MMR vaccine.
There is no need to delay getting immunized because of a cold or other mild illness. However, if you have concerns, speak with your health care provider.
Disease quick facts
- Measles
-
What is measles?
Measles is a serious illness caused by the measles virus. Measles is very contagious.Because of immunization, measles is now a rare disease in Canada. Most cases occur in unimmunized people, including visitors to Canada who have traveled overseas.How does it spread?
Measles is very contagious and spreads easily. The virus spreads through the air when an infected person breathes, coughs, or sneezes. The measles virus can survive in small droplets in the air for several hours. You can become infected when you breathe in these droplets or touch objects contaminated with the virus. The airborne spread of the measles virus makes the disease very contagious. Sharing food, drinks or cigarettes, or kissing someone who has the virus can also put you at risk.What are the symptoms?
Symptoms of measles include fever, cough, runny nose, and red and inflamed eyes that are often sensitive to light. These symptoms are followed by a rash, which starts first on the face and neck and spreads to the chest, arms and legs. The rash lasts about 4 to 7 days. There may also be small white spots inside the mouth. Symptoms can start as soon as 7 days after a person is infected with the measles virus.What are the risks of the disease?
Measles can cause encephalitis, an inflammation of the brain, which can lead to seizures, deafness, or brain damage. One out of every 3,000 people with measles may die from complications. Complications and death are most common in infants less than 12 months of age and adults.Complications of measles can include:- Ear infections
- Diarrhea
- Pneumonia
- Encephalitis (1 in every 1,000 cases)
- Mumps
-
What is mumps?
Mumps is a disease caused by the mumps virus. Mumps was a common childhood disease before immunization. It is now more common in young adults.How does it spread?
Mumps is very contagious and spreads easily. Mumps is spread by contact with saliva or mucus from an infected person's mouth, nose, or throat. When an infected person coughs or sneezes, the virus spreads through droplets in the air. You can be exposed to the virus even if you are 2 meters away from someone with mumps. You can become infected when you breathe in these droplets or touch objects and surfaces contaminated with the virus. Sharing food, drinks, or cigarettes or kissing someone who has the virus can also put you at risk.What are the symptoms?
Symptoms may include fever, sore muscles, headache and swelling of the salivary glands, especially the parotid glands that are at the side of the cheeks.Up to 30% of people with mumps do not have any symptoms. But they can still spread the mumps virus to other people.Symptoms can appear from 12 to 25 days after mumps virus infection.What are the risks of the disease?
Mumps can cause encephalitis, an inflammation of the brain that can lead to seizures or brain damage. About 1 in 20 people with mumps get mumps meningitis, an infection of the lining of the brain.Mumps can also cause temporary deafness. Permanent deafness occurs in less than 1 in 20,000 people who get mumps.Adults and teens with mumps can have painful swelling of the testicles (about 1 in 4 cases) or ovaries (about 1 in 20 cases). Both of these conditions are temporary and rarely result in permanent damage or sterility.Mumps infection in the early stage of pregnancy may increase the rate of miscarriage but has not been shown to cause birth defects. - Rubella
-
What is rubella?
Rubella, also known as German measles, is a disease caused by the rubella virus. Rubella is usually a mild illness but can be very serious for pregnant women and their developing babies.How does it spread?
Rubella is spread by contact with saliva or mucus from the mouth, nose or throat of an infected person. When an infected person coughs or sneezes, the virus spreads through droplets in the air. You can become infected when you breathe in these droplets or touch objects contaminated with the virus. Sharing food, drinks, or cigarettes or kissing someone who has the virus can also put you at risk.What are the symptoms?
Symptoms may include a rash, fever, joint aches, headache, discomfort, runny nose and irritated eyes. The lymph nodes located behind the ears and at the back of the neck may swell and feel painful.The rash, which may be itchy, begins first on the face and then moves downwards from the head to the feet and lasts about 3 to 5 days. About half of all rubella infections show no symptoms of a rash.Symptoms can appear 14 to 21 days after a person is infected with the rubella virus. In most cases, symptoms appear 14 to 17 days after exposure to the virus.What are the risks of the disease?
Rubella is usually a mild illness but can be very serious for pregnant people and their developing babies. If a pregnant person contracts rubella, they may have a miscarriage or stillbirth. Their baby may be born with severe birth defects, including deafness, eye problems, heart defects, liver, spleen and brain damage. This is called Congenital Rubella Syndrome (CRS). CRS occurs in about 9 out of 10 babies born to people who have rubella infection in the first 3 months of pregnancy. CRS is rare because so many people are immune to rubella infection due to routine immunization. Cases still occur in Canada, however, in babies born to people who immigrate to Canada as rubella immunization is not routine in many parts of the world.